COSENTYX® CONNECT
What is COSENTYX® Connect?
COSENTYX® Connect is a
support program designed to make onboarding
seamless and efficient for patients
and HCPs by providing helpful services:

Benefits verification
Investigate coverage obstacles and take action
Obstacles may include lack of coverage, prior authorization (PA) denial, or step therapy
Facilitate the PA process
Help initiate PA requests or letters of appeal directly with your office and/or have your office follow up with your patient's health plan regarding PA status
Many health plans will allow up to 3 levels of appeal of PA denials

Savings options
- Co-Pay* offer for eligible† privately insured patients
- Up to 2 years of FREE COSENTYX with Covered Until You’re Covered‡ if coverage is denied for eligible† privately insured patients during the appeals process

Pharmacy and patient partner
Assist with specialty pharmacy processing and delivery
- Once approved, transfer the prescription to the preferred or health plan–mandated specialty pharmacy for processing and delivery
- Work directly with the specialty pharmacy and patient to ensure delivery in a timely manner
- Contact the patient via phone call or text message

Continued
support
Provide
ongoing patient support services, tools, and resources
- Dedicated support from the COSENTYX® Connect team
- Welcome kit
- Optional travel bag and sharps container
- Online injection videos
- Timely emails and text messages based on patient contact preferences
*Limitations apply. Valid only for those with private insurance. Program provides up to $16,000 annually for the cost of COSENTYX and up to $150 per infusion (up to $1,950 annually) for the cost of administration. Co-pay support for infusion administration cost not available in Rhode Island or Massachusetts. Offer not valid under Medicare, Medicaid, or any other federal or state program. Novartis reserves the right to rescind, revoke, or amend this program without notice. See complete Terms & Conditions for details.
†Certain payers have carve-outs that restrict utilization of manufacturer support programs.
‡The Covered Until You’re The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to 2 years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
HCP, healthcare professional; PA, prior authorization.
What is the Start Form?
The Start Form coordinates patient insurance coverage for, access to, and receipt of COSENTYX. It also serves as an enrollment channel for the patient into COSENTYX® Connect and the Covered Until You’re Covered Program.* The Start Form requires important information that must be filled out by both the HCP and the patient, which includes the patient’s prescription, patient insurance, and patient and HCP signatures.
An electronic Start Form is available through CoverMyMeds.
If you have questions about the Start Form, please contact your Access & Reimbursement Manager (ARM) or call 1-844-COSENTYX (1-844-267-3689).
Start Form*The Covered Until You’re The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to 2 years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
HCP, healthcare professional.
What is CoverMyMeds®?

CoverMyMeds is a free healthcare service that provides prescription decision support, electronic prior authorization (ePA), and specialty support services.
COSENTYX has partnered with CoverMyMeds to create a convenient way to get patients started on the SC form of COSENTYX. Log in to covermymeds.com to submit and follow up on an ePA. Health plans typically make decisions within 3 days. If the health plan denies the PA, you can send an electronic Start Form through CoverMyMeds to enroll qualified* privately insured patients in our Covered Until You’re Covered Program.†
To learn more, click the CoverMyMeds bar on the
Getting Started With
SC page.
If you’d like an account, it’s easy to open one
online.
*Certain payers have carve-outs that restrict utilization of manufacturer support programs.
†The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to 2 years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
PA, prior authorization.
CoverMyMeds is a registered trademark of CoverMyMeds LLC. All rights reserved.
What is an Access & Reimbursement Manager (ARM) and how can they help me?

COSENTYX ARMs are experienced professionals with strong knowledge of the insurance landscape, who work with the COSENTYX® Connect team and your office to help navigate your patients’ health plan coverage.
ARMs can support your office by:
-
Addressing local and regional insurance landscape and coverage obstacles
-
Serving as a liaison between the customer and COSENTYX® Connect throughout the reimbursement journey
-
Educating customers about COSENTYX® Connect and product access process
SAVINGS OPTIONS
How can patients on the SC form of COSENTYX sign up for the Co-Pay offer?

The Co-Pay offer* helps your eligible† privately insured patients save on their out-of-pocket expenses for their treatment. This could allow your eligible patients to pay $0 for COSENTYX. In fact, 94% of enrollees paid NOTHING out of pocket.1 Patients may start saving today when they sign up for COSENTYX® Connect. To activate their co-pay savings, complete the Start Form (patients must sign and date) or have them sign up at the link below or call 1-844-COSENTYX (1-844-267-3689) and press option 1.
Once a patient has signed up for the Co-Pay offer, they do not have to sign up each year as long as their insurance has not changed.
Co-Pay* offer for eligible† SC patients to self-enroll*Limitations apply. Valid only for those with private insurance. Program provides up to $16,000 annually for the cost of COSENTYX and up to $150 per infusion (up to $1,950 annually) for the cost of administration. Co-pay support for infusion administration cost not available in Rhode Island or Massachusetts. Offer not valid under Medicare, Medicaid, or any other federal or state program. Novartis reserves the right to rescind, revoke, or amend this program without notice. See complete Terms & Conditions for details.
†Certain payers have carve-outs that restrict utilization of manufacturer support programs.
Reference: 1. Data on file. Cosentyx Co-pay Program Data. Novartis Pharmaceuticals Corp; March 2023.
Is there a bridge program for patients who are not initially covered for COSENTYX through their private insurance?

Yes, the Covered Until You’re Covered Program provides up to 2 years of FREE COSENTYX if coverage is denied for qualified*† privately insured patients during the appeals process.
See how Covered Until You’re Covered helps patients overcome common coverage challenges and next steps to get patients started:
Navigating SC Access Top Challenges*Certain payers have carve-outs that restrict utilization of manufacturer support programs.
†The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to 2 years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
What is the Covered Until You’re
Covered
Program?

The Covered Until You’re Covered Program provides up to 2 years of FREE COSENTYX if coverage is denied for qualified*† privately insured patients during the appeals process.
See how Covered Until You’re Covered helps patients overcome common coverage challenges and next steps to get patients started:
Navigating SC Access Top Challenges*The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to 2 years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
†Certain payers have carve-outs that restrict utilization of manufacturer support programs.
INSURANCE COVERAGE
Does my patient’s health plan
cover
COSENTYX?
Write COSENTYX. Get COSENTYX. COSENTYX is included on most formularies for privately insured patients.1* Check the health plan’s coverage details by calling or visiting them online. If you have questions about specific plans and coverage tiers, your COSENTYX Access & Reimbursement Manager (ARM) or Sales Representative can help. Get in touch here.
*COSENTYX is present on formularies as either a first-, second-, third-, fourth-, or fifth-line biologic. Novartis does not guarantee payment or coverage for any product or service. Actual coverage and reimbursement decisions are made by individual payers following the receipt of claims. Coverage information is subject to change by the relevant payer.
Reference: 1. Data on file. Cosentyx Access. Novartis Pharmaceuticals Corp; July 2023.
How can I help patients get started
on
COSENTYX?
There are 3 fast and convenient ways to get patients started on COSENTYX:
-
Through your CoverMyMeds (CMM) account—upon submission of the electronic Start Form, CMM will complete PA requests, automatically enroll patients in COSENTYX® Connect, and transfer the prescription to the patient’s health plan–preferred specialty pharmacy for delivery once approved
-
Directly with a Specialty Pharmacy—all specialty pharmacies can fill a prescription for COSENTYX. Pharmacists often coordinate the PA and appeals process, work with the office to gain approval, and can transfer the prescription to the patient’s health plan–preferred pharmacy, if required
-
Through COSENTYX® Connect—once the completed Start Form has been received, the COSENTYX® Connect team will conduct a benefits verification and provide support throughout the PA and appeals process
Choose the channel that’s right for your office. Most prescriptions receive PA approval the first time around. See the Getting Started With SC page for more information about each onboarding pathway.
How do I appeal to my patient’s health plan if the prior authorization (PA) or exception request has been denied?
If an exception request or PA is denied, the patient’s health plan will provide a written explanation as to why it was denied and include information about how to request an appeal. Your office may file an appeal on the patient’s behalf.
An appeal is a request to the patient’s insurance company to reconsider their decision to deny coverage of COSENTYX. Appropriate documentation, such as an appeal letter, letter of medical necessity, and relevant medical records can/should be submitted.
We are here to help. If you have questions, please contact your Access & Reimbursement Manager (ARM) or call the COSENTYX® Connect team at 1-844-COSENTYX (1-844-267-3689).
For additional information, a helpful appeal submission checklist, and sample appeal letters, download our Prior Authorizations, Exceptions & Appeals Kit:
What should I do if my patient’s health plan
no longer covers COSENTYX?
Most health plans have a list of preferred and covered medications called a formulary. This list may be reevaluated every year based on a number of factors, including cost, safety, and effectiveness of the medication. A health plan may decide to remove COSENTYX from their formulary and exclude it from coverage, which causes patients to experience a nonmedical switch to another medication. Nonmedical switching involves a change in medication in a patient who typically is stable on their prescribed medication often for insurer cost-saving reasons, rather than for reasons related to effectiveness or safety.1
If a patient and the prescriber wish to continue with COSENTYX, you may submit an exception request on the patient’s behalf. Download our Prior Authorizations, Exceptions & Appeals Kit below for additional information, a submission checklist, and sample Letters of Medical Necessity when submitting an exception request.
We are here to help. If you have any questions, please contact your Access & Reimbursement Manager (ARM) or call the COSENTYX® Connect team at 1-844-COSENTYX (1-844-267-3689).
Reference: 1. Costa OS, Salam T, Duhig A, et al. Specialist physician perspectives on non-medical switching of prescription medications. J Mark Access Health Policy. 2020;8(1):1738637.
What is a medical exception?
A medical exception request is a way to ask a health plan to reconsider a formulary decision with respect to an individual patient for medical reasons. The prescriber must submit a statement of medical necessity with supporting information describing why COSENTYX is preferred over the health plan–mandated treatment option.
Download our Prior Authorizations, Exceptions & Appeals Kit below for additional information, a submission checklist, and sample Letters of Medical Necessity when submitting an exception request.
We are here to help. If you have any questions, please contact your Access & Reimbursement Manager (ARM) or call the COSENTYX® Connect team at 1-844-COSENTYX (1-844-267-3689).
How can I help if a patient is having
trouble
refilling their prescription?
If a patient is having issues refilling their COSENTYX prescription, they may be out of refills or the prior authorization (PA) from their health plan may have expired. Ask the patient to check with their pharmacy for more information and let you know what they learn. You may need to provide a new prescription and/or process another PA. Remind the patient to make a note of their PA approval and number of refills for future reference.
STARTING COSENTYX
Where can I find a list of contacts that are available to support my office and patients?
See our Important Contacts page for a list of resources and their available links, phone numbers, and fax numbers that may be useful when helping patients start and stay on COSENTYX.
How can I provide patients with more
information about their disease?
Patients can use one of the COSENTYX patient brochures to learn more about their disease and how COSENTYX can help them take control of their disease.
How can I provide patients with
more information about COSENTYX?
Patients can use one of the COSENTYX patient brochures to learn more about how COSENTYX can help them take control of their disease. For additional information about COSENTYX, patients can also visit www.COSENTYX.com.
How can I find dosing information
for
the SC form of COSENTYX?
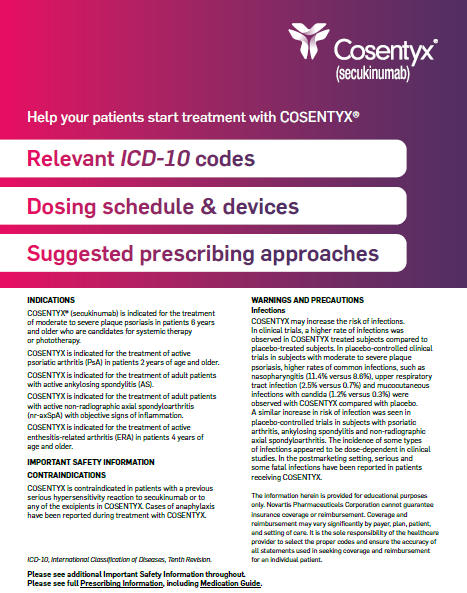
Please review the ICD-10 Coding & SC Dosing resource below for relevant ICD-10 codes, information about injection devices, and the dosing schedule and suggested prescribing approaches for the SC form of COSENTYX.
ICD-10 Coding & SC DosingICD-10, International Classification of Diseases, Tenth Revision.
Are there injection resources available
for patients on the SC form
of
COSENTYX?
Patients who need a little extra help with their self-injections can access step-by-step injection demonstrations via our injection video library and explore other helpful injection resources:
Where can I learn more about the results of treatment with COSENTYX in clinical trials?
Please visit COSENTYXhcp.com to learn more about how the SC form of COSENTYX performed in clinical trials.
What testing do patients need to
complete before starting COSENTYX?
Evaluate patients for tuberculosis (TB) infection prior to initiating treatment with COSENTYX. Please see the full Prescribing Information for more information about pretreatment evaluation for tuberculosis.
For additional resources, please visit the
Important
Contacts page or contact your Access
& Reimbursement Manager.
3/24 304256



